Physical Wellness
Exercise and eating nutritiously, yes, but what else can play a role?
In a previous newsletter, we talked about the six dimensions of wellness and how they apply to your goal of aging well. Today, we will discuss the first dimension, physical wellness, in more detail. Then, in future newsletters, we will address the other dimensions as shown below.
Physical wellness promotes proper care of the body for optimal health and functioning. In a recent study, researchers analyzed the exercise, functional limitations, excess weight, self-perceived health status, and chronic health problems in the over 65 population. The researchers found that those folks were becoming increasingly less physically active. There is good news, however! Even if your lifestyle has been inactive, it is never too late to change.
Making an exercise plan is a good idea. Such a plan can keep you on track and help you maintain focus on your goals. The plan should include walking, light exercise, and strength training, as well as balance and flexibility exercises. Although you may experience aches and pains at first, being active and more than a “couch potato” is a primary factor in pursuing physical wellness. Pinterest provides a good example of such a plan.
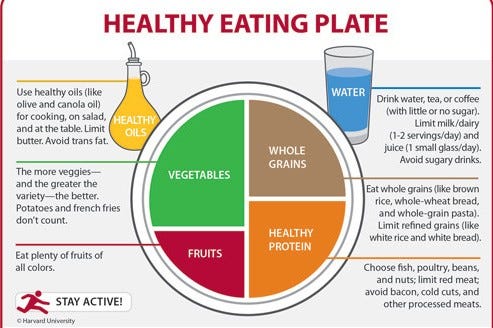
Eating nutritiously is just as important as exercise in helping people to manage their weight and keep themselves energized. Eating nutritiously lowers the risk of developing chronic health conditions such as heart disease and diabetes. During the past 30 years, the number of overweight older adults has doubled at an alarming rate. One plan for healthy eating is offered by Harvard University.
Much has been written about the need for older people to be physically fit and to eat nutritiously. You can read numerous articles online. So, in this newsletter I want to discuss other factors that play a role. Factors such as smoking cigarettes or pot, drinking too much alcohol, misusing prescription drugs, and staying in the hospital. So, let’s take a closer look at each of them.
SMOKING
The first factor I want to mention is cigarette smoking. Cigarette smoking is the leading cause of preventable disease and death in the United States. Smoking accounts for approximately 1 in 5 deaths every year. In 2016, an estimated 37.8 million adults in the United States smoked cigarettes and more than 16 million Americans lived with a smoking-related disease such as asthma or emphysema. According to the NIH
The disease consequence of smoking occurs disproportionately among the elderly because of the typically long duration of cumulative injury or change that underlies the bulk of tobacco-caused disease. Older smokers are less likely than younger smokers to attempt quitting, but they are more likely to be successful in the attempts they do make to quit. Excess absolute rates of disease incidence and mortality due to smoking increase steadily with increasing age and duration of smoking, and there is little evidence to suggest that the disease consequences of smoking diminish among the elderly.
Lung cancer is the largest cause of smoking-related deaths for people over the age of 60.
Approximately 70% of the 400,000 or more deaths occur among those over age 60 years. The benefits of stopping were somewhat less among the elderly and manifested more slowly than among younger smokers; however, to stop remains the most effective way of altering smoking-induced disease risks at all ages.
My Dad smoked cigarettes for 50 years and died of emphysema at age 71. I never smoked and have already outlived him by ten years. I’m not saying smoking was the sole cause of his death, but it was a contributor.
Then there is marijuana use. One research study suggested that the greatest increase in marijuana use was observed among people age 65 or older. Many used marijuana medicinally rather than recreationally. However, that may change as more states legalize marijuana use. A A Harvard blog notes that
According to a recent study in the Journal of the American Medical Association, cannabis use among older adults (defined as 65 and older) in the US has been steadily increasing. In this study, the prevalence of past-year use increased from 2.4% to 4.2% from 2015 to 2018. This study is consistent with other research, as well as with reports from physicians who recommend cannabis in their daily practices.
A 2014 review of marijuana use by older people pointed out that drowsiness and dizziness were known side effects of marijuana. Both side effects can contribute to an older person’s risk of falling. The review also pointed to an increased risk of irregular heart beat.
Other side effects of smoking marijuana include cardiovascular and respiratory problems which aare especially dangerous for the elderly. Cardiovascular effects such as a faster heartbeat and high blood pressure. It is also known that cannabis smoke is more irritating and more likely to cause cancer in the bronchial tubes than tobacco smoke.
ALCOHOL
The second factor I want to mention is alcohol consumption. Alcohol acts differently in older people than in younger people. Older folks may experience effects without increasing the amount of alcohol they drink, which in turn makes them more susceptible to accidents and falls. It is also known that older women may be more sensitive than older men to the effects of alcohol.
Drinking too much alcohol over a long period of time can lead to cancer, liver damage, immune system disorders, and brain damage. Excessive drinking can also worsen certain health conditions such as osteoporosis, diabetes, high blood pressure, ulcers, memory loss and mood disorders.
Drinking can make medical problems more difficult for doctors to find and treat. For example, alcohol causes changes in the heart and blood vessels; changes which can dull pain that may be a warning. Finally, too much alcohol can cause older people to be forgetful and confused: symptoms that can be mistaken for signs of dementia.
Click here to listen to Ellen’s story.
PRESCRIPTION DRUGS
The third factor I want to mention is the misuse or overuse of prescription drugs. While there is certainly a time and need for medication, it can and may be over prescribed. Think about this:
The statistics on medication usage among elderly patients in the US are eye-opening: more than one-third of prescriptions drugs used in the US are taken by elders. The average elderly patient has more than five prescriptions. The average nursing home patient has more than seven.
Pain is more prevalent in older people and the use of opiates for pain management can be an issue.
As people approach retirement, various life changes can lead to an increase in prescription drug abuse. Older adults have an increased likelihood of experiencing pain and physical illness and are prescribed pain relievers more frequently than younger people.
As we age, physiological changes occur and we metabolize alcohol and drugs at a slower rate. As such, an older individual will experience their effects more intensely and for a longer period of time than younger people. Older patients are likely to be prescribed multiple pain relievers which increases the severity of the side effects caused by opioids.
My husband’s reaction to the anesthesia and medications given during a 9-day hospital stay seems to be a prime example. He had slight memory problems and he was an older adult who took no prescription drugs prior to surgery. He exercised, ate well, held a job after he retired, and got together with friends. After the surgery, his memory declined significantly and never recovered. Recently, he was diagnosed with dementia and had to be placed in a memory care facility.
HOSPITAL STAYS
Which brings me to the final factor. Hospital stays can be stressful—for both elderly patients and their families. And while the hospital is supposed to make people well, elderly patients sometimes come out worse off than they went in. Hospitals can be dangerous places for elderly patients. Read Janet’s story, which is similar to my husband’s.
The stress of a hospital stay can turn into a decline in an elderly patient's mental and physical health, slowing down their long-term recovery, well-being, and quality of life. A 2012 study from Neurology suggested that in elderly patients, cognitive declines more than double after a hospital stay, affecting patients' thinking and memory skills.
The website Housing For Seniors provides a great list of things to watch for. Click here to learn more.
In summary, there are things you can do besides exercising and eating nutritiously if your goal is to age well.



Interesting stuff. I was surprised to find out that the elderly and increased marijuana usage. I also think it is a key point that some of these things have increased risk for the elderly due to the risk of falling, which is a frequent cause leading to death in older people. And of course, the risk of hospital stays for the elderly is also not as widely recognized as it should be.